The Introduction of Diarrhea
Definition
Diarrhea means a change in the bowel habits marked by frequent passage of loose watery unformed stools. It may be an acute or chronic condition.
Clinical features
Frequent bowel movements, loose watery unformed stools, abdominal cramping and pain and urgency of defecation, poor appetite, nausea and vomiting. Dehydration and imbalance of electrolytes are potential complications.
Correspondence to Western diseases
- Gastrointestinal disorders.
- Enteritis.
- Intestinal tuberculosis (TB is usually seen in the Lungs, but it can also invade the lymph nodes and move to the intestines).
- Functional disturbance of the intestines (e.g. Irritable bowel syndrome).
- Food poisoning.
The Etiology of Diarrhea
- Invasion of EPFs, especially Cold, Damp, Summer Heat, and Heat, (“stomach flu” is usually considered a Dampness invasion of the Spleen).
- Improper diet → food retention:
- Sweet fatty foods in people with a weak Spleen.
- Fatty foods are digested slowly, so they easily stay in the stomach too long.
- Cold raw food in someone with Spleen-Yang deficiency.
- Emotional frustration → Liver-Qi stagnation → Liver overacting on Spleen and Stomach.
- Weak constitution:
- Due to long-term illness, especially illness of the gastrointestinal tract.
- Chronic diarrhea damages the Spleen and Stomach.
- Kidney-Yang deficiency leads to early morning diarrhea.
The pathology of Diarrhea
Chief pathology
- Spleen Qi deficiency with Damp retention.
Chief pathological factors
- Dampness.
Chief organs involved
- Spleen and Stomach.
Related organs
- Liver (Liver-Qi stagnation).
- Kidney (Kidney-Yang deficiency diarrhea).
How to Diagnose and differentiate Diarrhea(see Table 10)
- Dampness.
Chief organs involved
- Spleen and Stomach.
Related organs
- Liver (Liver-Qi stagnation).
- Kidney (Kidney-Yang deficiency diarrhea).
How to Diagnose and differentiate Diarrhea(see Table 10)
- Liver (Liver-Qi stagnation).
- Kidney (Kidney-Yang deficiency diarrhea).
How to Diagnose and differentiate Diarrhea(see Table 10)
Tips for differentiation of patterns
(1)Differentiating excess from deficiency
Excess:
- Acute onset, short duration.
- Frequent bowel movements.
Deficiency:
- Slow onset, long duration.
- Diarrhea comes and goes.
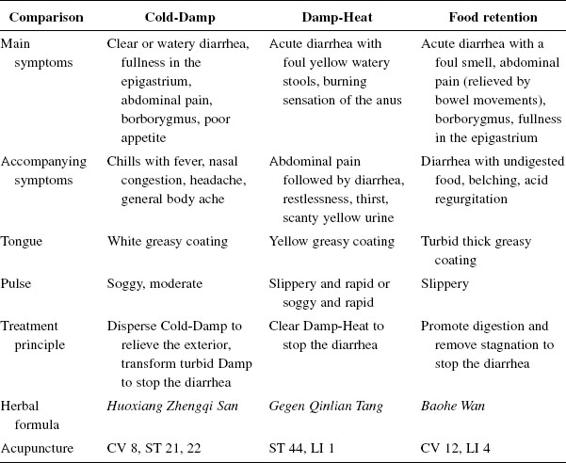
(2)Differentiation based on stools
- Watery diarrhea with fishy smell → Cold-Damp syndrome.
- Loose stools, brown in color, foul smell, burning around the anus → Damp-Heat syndrome.
- Loose stools, smell of rotten eggs, undigested food → food retention.
(3)Differentiation based on abdominal pain
- Distending abdominal pain that is relieved after a bowel movement but soon returns → food retention.
- Abdominal pain, borborygmus, urgent need for bowel movements, and afterward pain does not decrease and may be worse → Liver-Qi overacting on the Spleen.
- Cold pain in the lower abdomen, borborygmus, pain relieved by pressure and warmth → deficiency Cold.
- Urgent diarrhea with a burning sensation, abdominal pain, urgent need for bowel movements, explosive diarrhea → Heat syndrome.
Basic points: ST 25, 37, 36.
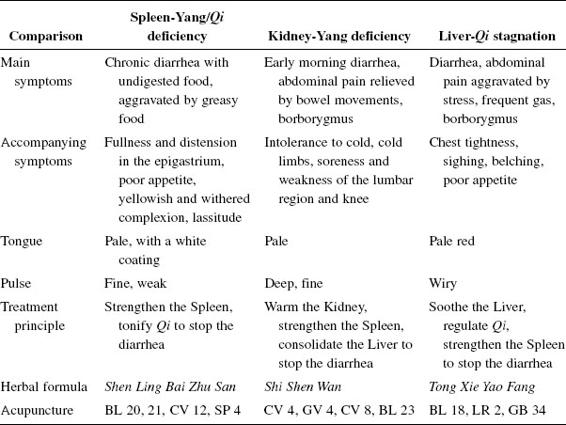
(4)Differentiating Zang-Fu organs for chronic diarrhea
- Diarrhea on and off with fatigue, often triggered by improper diet or overwork → Spleen-Qi deficiency.
- Diarrhea on and off, triggered by stress → the Liver overacting on the Spleen.
- Early morning (5–6 a.m.) diarrhea with undigested food, low back pain, and a feeling of coldness → Kidney-Yang deficiency or both Kidney and Spleen deficiency.
The Treatment of Diarrhea
Principles of treatment
- Tonify the Spleen.
- Remove Dampness.
(1)Modifications
- For acute diarrhea, focus more on removing Damp.
- For chronic diarrhea, focus more on tonifying the Spleen.
- If the Liver is involved, soothe it.
- If the Kidney is involved, warm it.
Herbal treatment
- Astringent herbals consolidate liquids (sweat, urine, stools) and can stop diarrhea, but be careful about using them too early in the treatment because they can also consolidate pathogenic factors (“close the door” and do not allow the pathogenic factor to escape).
- For chronic diarrhea, the pathogenic factor is almost gone and you need to promote Zheng Qi. Herbs to increase urination are often used, because they dry the stools, but if urination is promoted too much the Zheng Qi may get damaged.
Acupuncture
(1)Main points
- ST 25, 37, 36
(2)Acute
- ST 25, SP 9, ST 37
(3)Chronic
- CV 12, LR 13, ST 25, 36
(4)Severe heat
- ST 44 (Ying Spring)
- LI 1 (bleed)
- SI 1 (bleed)
(5)Modification by symptoms
Abdominal pain → LI 4.
Fullness in the epigastric region → SP 4.
Hypochondriac pain → GB 34.
Shortness of breath → CV 6.
(6)Diarrhea with cold limbs and a hidden pulse
- CV 8 (moxa with ginger to tonify Yang).
Moxibustion
(1)Main points
- ST 25
- CV 4
- CV 8
Use Moxa sticks for about 15 min or moxa coins (3–5 coins).
Auricular therapy
- Large Intestine
- Small Intestine
- Stomach
- Spleen
- Liver
- Kidney
- Sympathetic
- Shenmen
Bleeding therapy
- ST 36 (He Sea of the Stomach)
- SP 4 (Luo-Connecting Point)
- ST 44 (Ying Spring; for removing Heat)
- ST 45 (Jing Well; for removing Heat)
Electroacupuncture
- Choose one or two pairs of points.
- ST 36 (He Sea of the Stomach)
- SP 4 (Luo-Connecting Point)
- ST 44 (Ying Spring; for removing Heat)
- ST 45 (Jing Well; for removing Heat)
Electroacupuncture
- Choose one or two pairs of points.
(1)Chronic
- Moderate, intermittent wave for 20 min.
(2)Acute
- Moderate, continuous wave for 30 min.
Other treatments
(1)Hot salt compress
For chronic, Cold-type diarrhea, place 500–1000 g of salt in a small bag. Then warm the bag and apply to the following points for 30–60 min:
- CV 8
- CV 4
- Stomach 25
Herbal application
Place garlic paste on K I1 or CV 8.
Suggestions
- Improper diet — Educate the patient about good food hygiene and about consuming less raw, cold, sweet, greasy food and less alcohol.
- Prevent EPF invasion, especially during summer.
- Regulate emotions to decrease stress.
- Have bed rest; keep warm; eat fresh, easily digested food; drink enough (but not too much) water, especially with some salt (salt cleanses the bowels and supplements electrolytes).

